Report of an online survey among health care workers in India
by Savithri Devi, Shrinidhi Datar, Subha Sri B
Introduction
While India is facing the COVID-19 pandemic, healthcare workers who are at the frontline of this situation are at severe risk of infection by the novel coronavirus. A significant measure to prevent this is use of Personal Protective Equipment (PPE). Several agencies like WHO and the MoHFW, GoI have put out guidelines regarding rational use of PPE. However, numerous media reports suggest shortage of PPE across different facilities in the country and also rising numbers of healthcare worker infections. This study was therefore carried out to understand the situation around PPE in India including its availability, status of training on PPE, and difficulties and concerns of health care workers regarding PPE. To our knowledge, this is the first systematic study to understand availability of PPE amongst health care workers in India.
Methodology
This study was cross-sectional in design and used a semi-quantitative survey methodology that was self-administered by different levels of health care workers using an online medium using Google form in two languages, English and Hindi. A telephonic survey was also built in wherein the researchers administered the form verbally over the phone to participants who prefer this. Respondents were invited through social media, e-groups, and through associations of different healthcare workers. As the survey was done through an online methodology, the sample of respondents was self-determined by those health care workers who chose to respond to online invitations. Thus, the sample was purposive. Data collection was done online between 06 and 18 May 2020.
Given the limitations of the online methodology and the practical difficulties due to the lockdown, the number of respondents is only a very small proportion of health care workers in India. Thus, the study provides an indication of the prevalent situation of PPE in different health care settings in the country.
Key findings
A total of 392 respondents participated in the online study. These included 155 doctors, 103 postgraduate residents and interns, 34 nurses and 27 Community Health Workers. More than half (229, 58.4%) worked in public sector facilities. The respondents were spread across 26 States and Union territories and more than 150 districts. More than 50% were from 3 states:
- Maharashtra (100),
- Tamil Nadu (58) and
- Madhya Pradesh (44).
Over half (212) belonged to Red Zone districts and nearly half (183) were working in designated COVID centres.
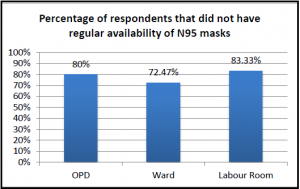 Almost all components of PPE were found to be either inadequately available or not available at all in most health care settings. Nearly a third of respondents working in OPD (43 of 135, 31.9%) reported that N95 masks were not available at all; only 27(20%) reported that they were regularly available in adequate quantities. Just over a quarter of respondents who worked in wards (21 of 76, 27.6%) reported that N95 masks were regularly available to them. Of those working in labour rooms (24), less than a third (7) reported regular availability of face shields. One in five working in Operation Theatres (4 of 20) reported that face shields were not available at all. Among 8 persons who reported working in ICU settings, only 4 reported regular availability of N95 masks in adequate quantities, 5 reported regular availability of gowns/coveralls, and 4 reported regular availability of goggles and face shields.
Almost all components of PPE were found to be either inadequately available or not available at all in most health care settings. Nearly a third of respondents working in OPD (43 of 135, 31.9%) reported that N95 masks were not available at all; only 27(20%) reported that they were regularly available in adequate quantities. Just over a quarter of respondents who worked in wards (21 of 76, 27.6%) reported that N95 masks were regularly available to them. Of those working in labour rooms (24), less than a third (7) reported regular availability of face shields. One in five working in Operation Theatres (4 of 20) reported that face shields were not available at all. Among 8 persons who reported working in ICU settings, only 4 reported regular availability of N95 masks in adequate quantities, 5 reported regular availability of gowns/coveralls, and 4 reported regular availability of goggles and face shields.
The situation was not different in public sector facilities or red zone districts. Over one in five of those working in red zone districts (46 of 212) reported that N95 masks were not available to them. Amongst those working in designated COVID centres, just over a third (68 of 183, 37.2%) responded that N95 masks were regularly available in adequate quantities.
Only a quarter of Community level health workers who were engaged in contact tracing and door to door surveys had regular availability of surgical masks, and less than a third (32.35%) had regular availability of gloves.
A significant proportion of health care workers (14%), including in red zone districts, reported purchasing their own PPE or receiving it in the form of donations from NGOs.
Over a third of all respondents (147 of 392, 37.5%) reported reusing their PPE, often without adequate disinfection practices recommended before reuse. WHO classifies extended use of PPE or reuse of PPE as “last-resort temporary measures in crisis situations to be adopted only where there might be serious shortages of PPE or in areas where PPE may not be available.” Even then, it cautions that “the reuse of any item without a reprocessing/decontamination process is considered inadequate and unsafe.”
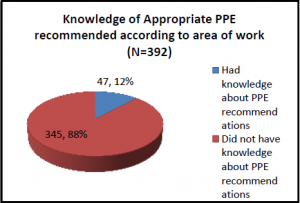 The study also found that a majority of respondents (345 of 392, 88%) did not have knowledge of appropriate PPE recommended as per their work setting. Over half of the respondents reported that they have not received any training regarding use of PPE, with one in five reporting that they were either self-taught or taught by peers and colleagues informally.
The study also found that a majority of respondents (345 of 392, 88%) did not have knowledge of appropriate PPE recommended as per their work setting. Over half of the respondents reported that they have not received any training regarding use of PPE, with one in five reporting that they were either self-taught or taught by peers and colleagues informally.
Over a third of the health care workers (138, 35.2%) expressed fear or concerns regarding use of PPE, its protective capacity, the risk of exposure to infection, and spreading it to their family members. Close to a half of all respondents (180 of 392, 45.92%) reported facing practical difficulties during working with PPE including sweating profusely, feeling hot, suffocated and dehydrated with long use of PPE, difficulties in performing medical procedures due to loss of dexterity, visual and auditory difficulties leading to difficulties in writing, auscultation or performing procedures, and practical difficulties like inability to eat, drink or use washrooms.
Over a third of all respondents (146 of 392, 37.2%) felt that there was discrimination in the process of distribution of PPE. Most of such perceived discrimination was related to PPE being distributed only to certain cadres hierarchically (e.g. doctors as opposed to nurses, senior doctors as opposed to interns), or to only certain departments in a facility being provided PPE while others were not.
Recommendations
1. Ensure adequate availability of PPE: The government must make available adequate PPE as per its guidelines at all health facilities in the public sector and bring regulations to ensure that healthcare workers in the private sector health facilities have access to appropriate PPE. It is also necessary to ensure such availability in ALL health facilities, including those at lower level and in non-hotspot areas, and in various health care settings, including at community level. The process of distribution of PPE must be transparent such that all healthcare workers receive appropriate PPE irrespective of the hierarchy of their cadre. Use of tools such as PPE burn rate calculator applications may be considered to assist calculating need and optimize rational use of PPE at institutional level.
2. Ensure training on PPE: Adequate training must be provided to all health care workers regarding PPE recommendations, its use, disposal, and reuse.
3. Addressing fears and concerns of health care workers: A grievance redress mechanism that includes an immediate response component should be set up for health care workers experiencing any difficulties in their work while managing patients with COVID. In addition, health care workers also need adequate mental health support to help them deal with fear, concerns, isolation and burnout they may be experiencing. This may be in the form of widely publicised mental health helplines, periodic institute level group therapy sessions, considerate work schedules, and “buddy” system of pairing healthcare workers together.
4. The need for systematic studies regarding situation of PPE in the country: In the situation of rising healthcare worker infection, it is required to assess the situation regarding availability, quality and use of PPE more thoroughly at regular intervals through research studies that are transparent and properly reported. . There have also been many modifications and innovations regarding PPE at some institutions and individual levels. There must be an attempt to standardize these innovations and scale up those that are found to have proven efficacy.
Details of the study
This study was conducted by Savithri Devi, Shrinidhi Datar, and Subha Sri B, who are independent medical doctors and public health researchers. Ethical approval for this research was provided by SOCHARA (Society for Community Health Awareness, Research and Action) Institutional and Scientific Committee (SISEC), Bengaluru, Karnataka. Dr Antony Kollannur, Dr Rakhal Gaitonde and Dr Prabir Chatterjee were advisors to the study.
The full report: kindly email to sairam1179@gmail.com.
For further details: please contact:
Dr. Savithri Devi
Phone: 7709350768
sairam1179@gmail.com
Dr. Subha Sri B
Phone: 9840260715
subhasrib@gmail.com